Blog
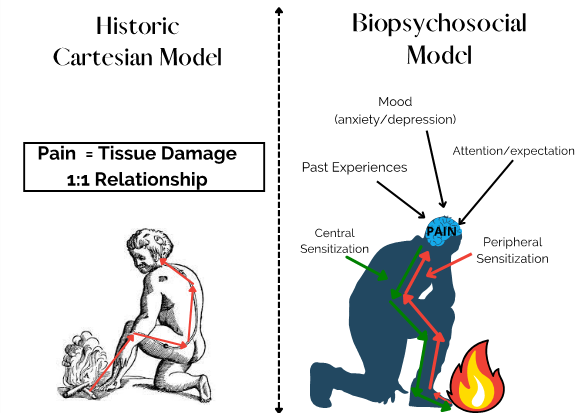
Understanding Pain- Part 1
By Camilla Noble What is pain? Pain is a complex experience and can be extremely overwhelming to navigate both as a clinician and patient. There is so much information out there but it can be hard to know where to start and who to go to when we need help looking for...
What is Craniosacral Therapy?
Craniosacral Therapy (CST) is a gentle, hands-on method of evaluating and enhancing the craniosacral system. The craniosacral system is a physiological system within the body. It is comprised of the structures that support the brain and the spinal cord, namely the...
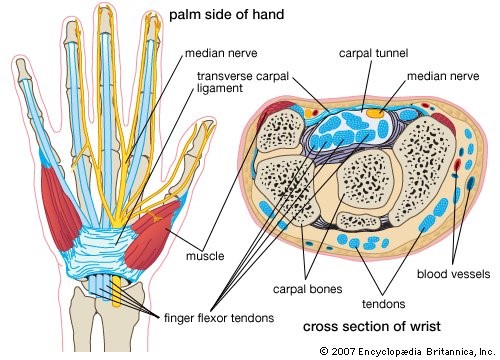
Carpal Tunnel Syndrome (CTS)
What exactly is CTS? It refers to a condition where the median nerve is being compressed at the level of the wrist as it runs through the carpal tunnel into the hand. The carpal tunnel is the passage way that connects the wrist and hand. It is formed by the carpal...
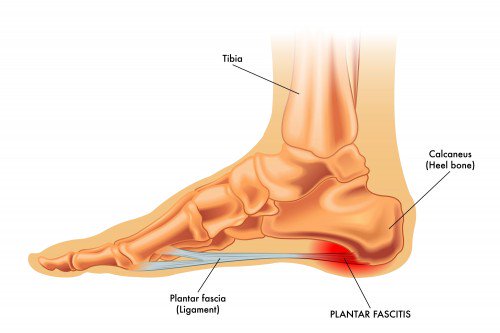
Do Physios treat plantar fasciitis?
Yes, we do. Out of a number of foot problems that we see, plantar fasciitis is a relatively common problem that Physios treat. Conservative treatment done by physios has a high success rate, even though it may take a few weeks or months to improve. The healing...
Do Physio’s treat sciatica?
The answer is a definite yes. In fact a recent study showed that starting Physio right away, rather than taking the usual watch and wait approach, helped improve the function and other outcomes for patients experiencing recent-onset back pain with sciatica (1). But...
Why you should join a Pilates class!
As we continue to live within the realities of COVID-19, some of us have needed to change the way we exercise. From joining online zoom classes, to building in more strength or mobility work – these are some of the positive changes “life at home” has brought with it....
Visceral Manipulation
What is Visceral Manipulation? Visceral Manipulation is a non-invasive therapy that requires extremely specific placement of gentle manual forces to encourage movement of the viscera (organs) and their surrounding connective tissue. In the words of Jean- Pierre...
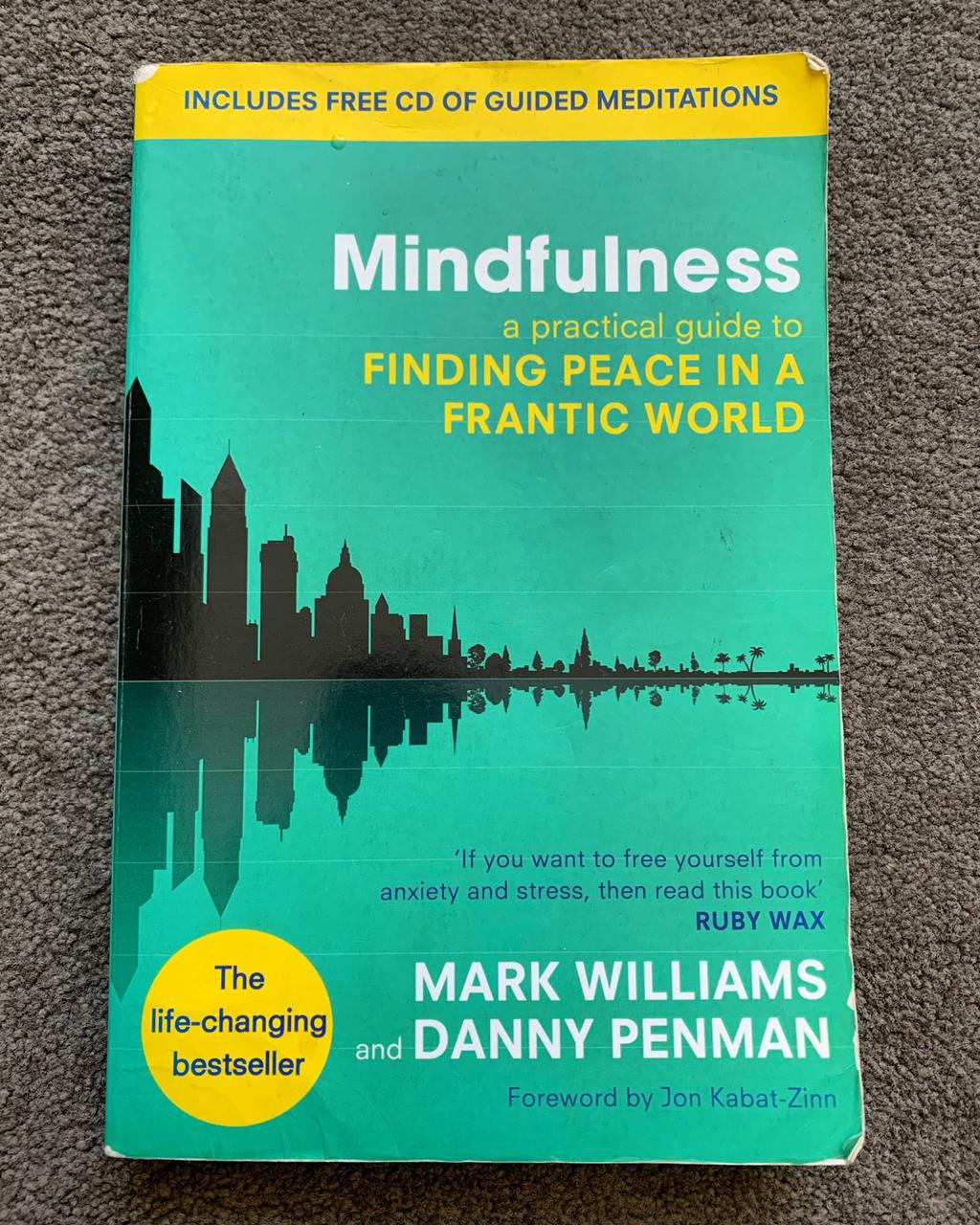
Mindfulness and Meditation
We’ve all heard these words a million times, but what do they actually mean? Is meditation just for Buddhists, hippies and yogis? Why is mindfulness important and how does a person implement it in their lives? I first started asking these questions about 4 years ago...
Why We Sleep
Sleep, a topic that thanks to the stress of the COVID-19 pandemic, has become all the more relevant. We have had an increasing number of clients in the practice reporting feelings of anxiety and being overwhelmed by many of the knock-on effects that this global...
Stress – The Good, the Bad and the Ugly!!!
I’d say it is safe to say that most people have experienced stress in their lives. The very act of being born is stressful for both mom and baby, no matter the circumstances. Take a look at the Oxford Dictionary’s definition of stress (as a noun): Pressure or tension...